In this blog post I want to explore some other topics related to VR or immersion therapy but from a bit of a different angle and with a more distant view on the core themes discussed thus far. So let us get rigth into it.
Redefining Healthcare in the Digital Age
In the fast-paced realm of modern healthcare, two terms have been gaining momentum: telehealth and digital therapeutics. As we navigate through a modern, digital landcape where technology intertwines with every aspect of our lives, it is very important to understand how these innovations are reshaping the landscape of healthcare delivery and patient treatment.
Understanding Telehealth and Digital Therapeutics
Let us start by dissecting these concepts. Telehealth encompasses a broad spectrum of healthcare services delivered remotely through telecommunications technology, i.e. remotely. From virtual doctor visits to remote patient monitoring, telehealth leverages digital platforms to bridge the gap between patients and healthcare providers, fostering accessibility and convenience.
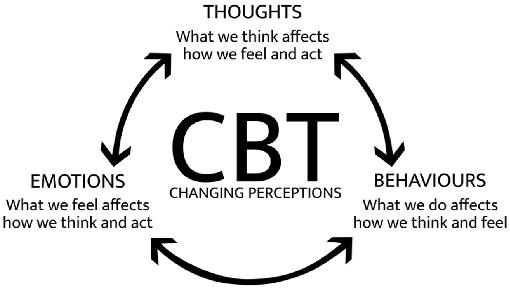
On the other hand, digital therapeutics (often shortened to DTx) represent a distinct category of healthcare treatments that utilize digital technologies to treat medical conditions or enhance clinical outcomes. Unlike traditional pharmaceuticals, digital therapeutics deliver evidence-based interventions through software programs or devices, often targeting behavioral changes or managing chronic diseases (which are also often times treated using immersion therapy).
Differentiating Between Telehealth and Digital Therapeutics
While both telehealth and digital therapeutics operate within the digital realm, they serve distinct purposes in the healthcare ecosystem. Telehealth primarily focuses on delivering clinical services remotely, facilitating consultations, diagnoses, and monitoring of patients‘ health status. In contrast, digital therapeutics delve deeper into the realm of treatment, offering interactive interventions tailored to manage specific health conditions or modify patient behaviors. In short Telehealth can be seen as virtual doctors visits whereas digital therapeutics simply means the ultilization of digital tools for therapeutic measures.
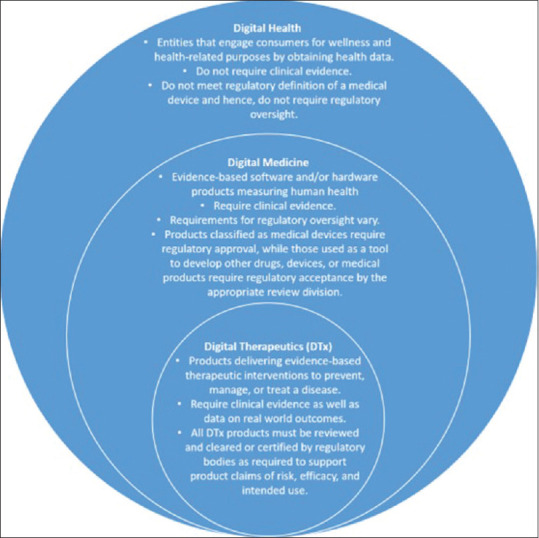
There are also the terms digital health and digital medicine floating around. For the sake of clarity I will mention a definition provided by [1] as seen in Figure 1.
Exploring Use Cases and Applications
The applications of telehealth and digital therapeutics are as diverse as the healthcare landscape itself. From remote consultations for routine check-ups to virtual sessions for mental health counseling, telehealth offers a huge variety of solutions to enhance patient access and streamline healthcare delivery. Patients can now seek medical advice from the comfort of their homes, minimizing travel time and reducing exposure to contagious illnesses. Furthermore, as previously mentioned in other blog posts, travel may not be enjoyable or even feasable for some patients. Receiving healthcare instructions remotely provides an important form of healthcare accessability. In Austria measures regarding telehealth have already been taken with ELGA (Elektronische Gesundheitsakte) which is a system that allows medical professionals and patients to view their medical files digitally.
Digital therapeutics, on the other hand, are chaning the treatment methods across various medical domains. From managing diabetes and cardiovascular diseases to addressing mental health disorders and addiction, digital therapeutics present new and novel approaches to enhance traditional treatments or serve as standalone interventions. One further positive aspect is that it can lead to increased patient engagement (improved frequency and regularity of treatments) due to the level of comfort and ease of use.
Bridging the Gap with Virtual Reality Therapy
As we delve deeper into the realm of digital therapeutics and telehealth solutions, the parallels with virtual reality (VR) therapy become apparent. Virtual reality therapy utilizes immersive technology to create therapeutic environments that simulate real-world scenarios and facilitate exposure-based treatments for mental health disorders, phobias, and PTSD (and many more). Patients can engage in virtual reality sessions guided by healthcare professionals, addressing psychological challenges and overcoming barriers to treatment through immersive simulations.
Summary & conclusion
In conclusion, telehealth and digital therapeutics represent a modern shift regarding the topic of healthcare. How and when we receive healthcare is being changed by these processes. By embracing digital innovations and leveraging the power of technology, we can enhance patient outcomes, improve accessibility, and revolutionize the healthcare experience for generations to come. Steps have and are being taken, but it will surely be a long and ongoing process until new technologies are fully utilized.
References used in this article and for research
https://gomohealth.com/2021/the-difference-between-digital-therapeutics-and-telehealth/
[1] J Family Med Prim Care. 2020 May; 9(5): 2207–2213.
very interesting paper on DTx which provides a great overview
https://www.apa.org/practice/digital-therapeutics-mobile-health
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5214969/
a paper about the impact of digital technology on the field of psychology especially
ELGA – die elektronische Gesundheitsakte | Gesundheitsportal